What is Breast Imaging?
– Breast imaging includes mammograms and ultrasound scans.
– Mammograms use low-dose X-rays to detect abnormalities.
– Ultrasound is radiation-free and distinguishes between solid and fluid-filled lumps.
– Dense breast tissue can complicate cancer detection.
– Early screening significantly lowers the risk of death from breast cancer.
Understanding Breast Imaging
Breast imaging involves creating images of breast tissue to screen for or diagnose conditions such as breast cancer. The two most common types are mammograms and breast ultrasound scans.
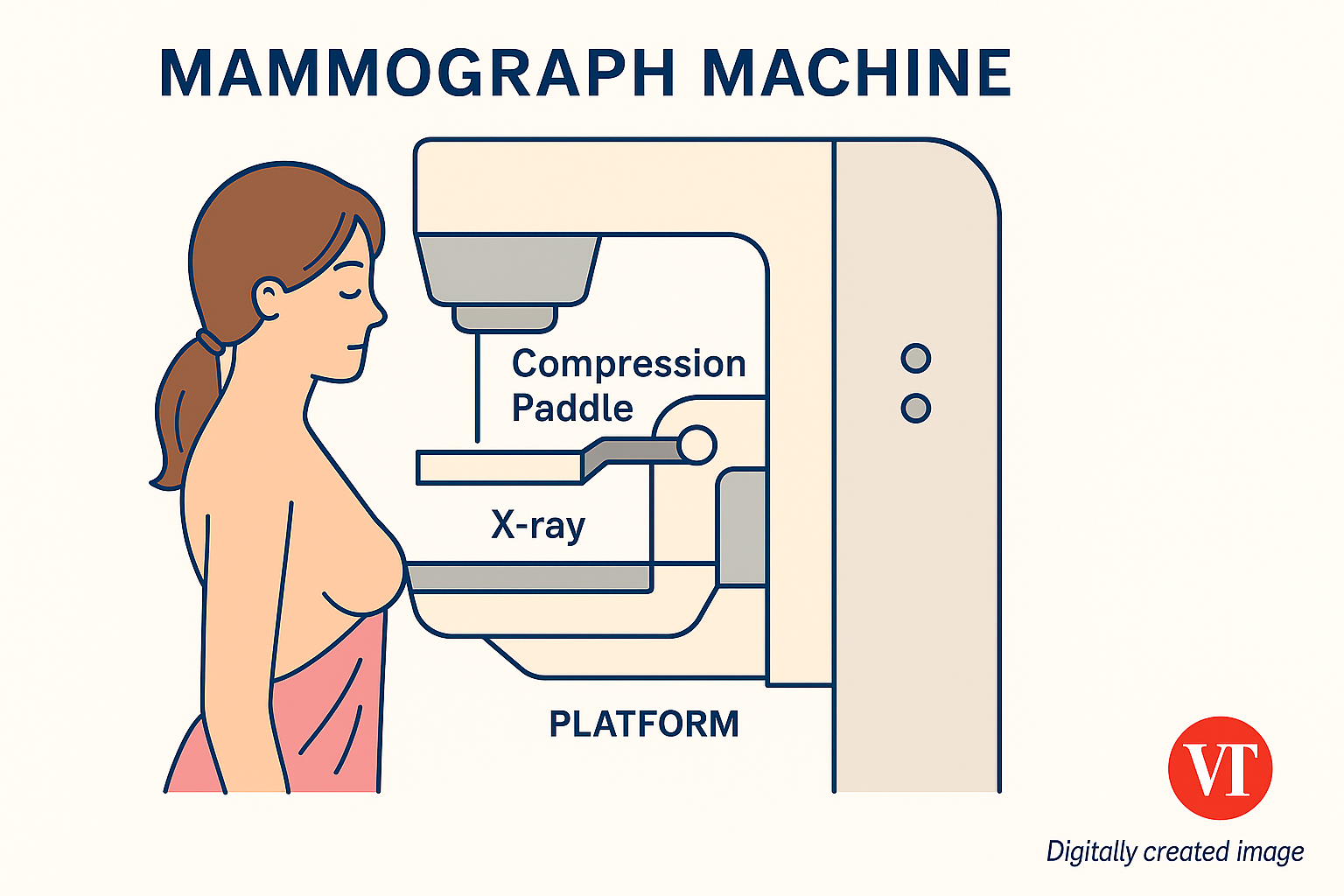
What is a Mammogram?
A mammogram uses low-dose X-rays to detect abnormalities in breast tissue. It is an essential tool for early breast cancer detection and diagnosis.

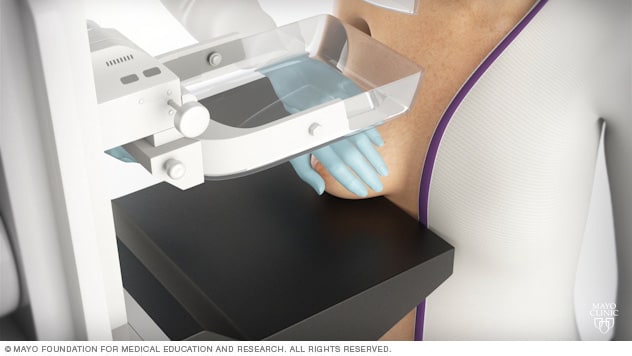
How is a Mammogram Performed?
The procedure involves placing the breast on a flat surface and compressing it with a paddle for 10 to 15 seconds. Patients stand during the scan. During a mammogram, patient stands in front of an X-ray machine designed for mammography. A technician places your breast on a platform and positions the platform to match your height. The technician helps you position your head, arms and torso to allow an unobstructed view of your breast.
What is a Breast Ultrasound Scan?
Ultrasound imaging uses high-frequency sound waves to capture images. It’s safe, non-invasive, and does not involve radiation. Often, it complements a mammogram to provide more detail.

Why is it Needed?
Ultrasounds are particularly useful for evaluating lumps and determining if they are solid or fluid-filled (e.g., benign cysts). This aids in prompt treatment.
How is it Performed?
During the scan, you lie on your back and raise your arm. A gel is applied to the breast, and a transducer is used to scan the area. The procedure lasts 30–60 minutes.
Preparing for a Mammogram or Ultrasound
- Schedule your exam 1 week post-menstruation to reduce discomfort.
- Inform the radiographer if you’re pregnant or may be pregnant.
- Wear a two-piece outfit as you’ll need to undress from the waist up.
- Avoid deodorant, perfume, lotion, or talcum powder on the day of the exam as these can affect imaging results.
Frequently Asked Questions
Am I at risk of getting breast cancer?
All women are at risk. Factors that increase risk include:
- Age – risk increases with age
- Family history of breast cancer
When should I go for breast imaging?
Seek medical advice if you experience:
- Breast pain or lumps
- Nipple or surrounding tissue changes
Mammogram guidelines:
- Yearly screening for ages 40–49
- Every two years if 50 and above
What are the Four Categories of Breast Density?
Levels of density are described using the American College of Radiology’s Breast Imaging Reporting and Data System (BI-RADS):
- A: Almost entirely fatty — very little dense tissue
- B: Scattered areas of fibroglandular density
- C: Heterogeneously dense — most tissue is dense
- D: Extremely dense — nearly all tissue is dense
You’re considered to have dense breasts if you fall into categories C or D. Around 50% of those screened do.
What Causes Breasts to Be Dense?
- Younger age
- Lower body fat percentage
- Hormone therapy for menopause
How Serious is Dense Breast Tissue?
- Increases the chance breast cancer might be missed on a mammogram
- Modestly increases the risk of breast cancer
How Often Should I Get a Mammogram if I Have Dense Breasts?
Screening is recommended annually from age 40 for most people. Having dense breasts may justify more frequent or additional screening tests like:
- 3D mammogram (Tomosynthesis)
- Breast MRI
- Ultrasound
- Contrast-enhanced digital mammogram
- Molecular breast imaging
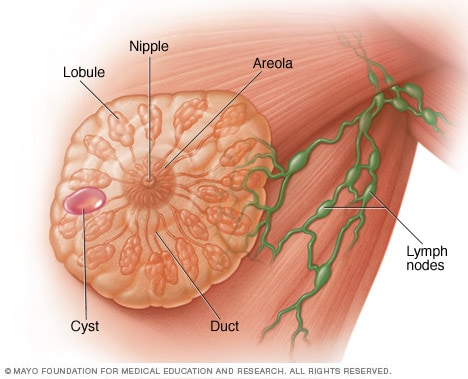
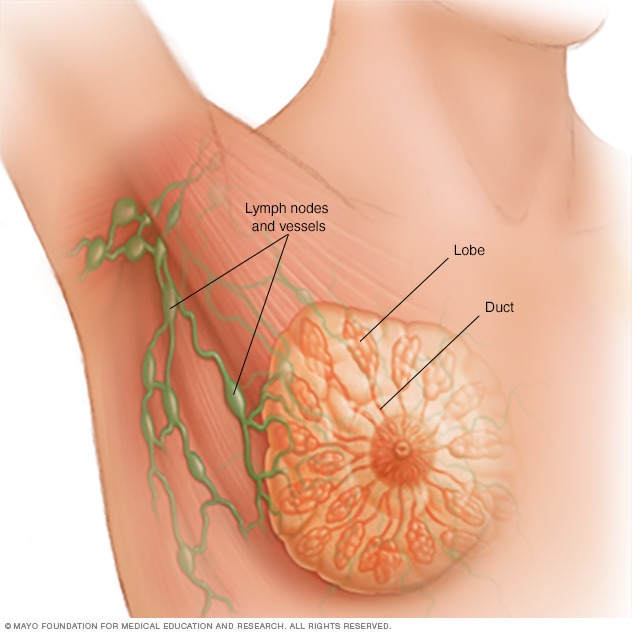
Breast Anatomy
Each breast contains 15 to 20 lobes of glandular tissue, arranged like the petals of a daisy. The lobes are further divided into smaller lobules that produce milk. Small tubes called ducts conduct the milk to a reservoir beneath the nipple.
Guidance from Mayo Clinic
Mayo Clinic recommends annual mammograms starting at age 40. Screening earlier may be particularly important for Black women due to higher risk and earlier onset.
Newer technology like 3D mammograms and digital imaging improves detection in dense breasts. False positives may occur but early detection outweighs the risks.
Talk to your healthcare team about your personal risks, screening options, and how often you should be tested based on your breast density and medical history.
Sources:
TTSH Breast Imaging,
Breast Imaging PDF,
Mayo Clinic
A global media for the latest news, entertainment, music fashion, and more.